The eyes are some of the most sensitive and vulnerable organs in the body. Airborne allergens and other particles can land directly on the surface of the eye, causing irritation and redness. Although tears constantly wash the eyes, they can’t always keep out allergens like pollen or pet dander. Because of this, allergies that flare up in the eyes, also known as ocular allergies, are common.
What Are Ocular Allergies?
Eye allergies are no different from allergies that affect your sinuses, nose or lungs. When an allergen comes in contact with your eyes, your body releases histamine – a chemical produced in reaction to a substance that the immune system can’t tolerate. Special cells called mast cells make histamine. These cells are present throughout the body but are highly concentrated in the eyes.
Location of allergy symptoms depends somewhat on where the allergen has come into contact with your body. Ocular allergens tend to be airborne (as are most other allergens).
The most frequent allergic triggers include:
- Pollen
- Pet hair or dander
- Dust
- Some medicines
There are also are some triggers that irritate the eyes but are not true allergies, such as:
- Cigarette smoke
- Perfume
- Diesel Exhaust
What Is Allergic Conjunctivitis?
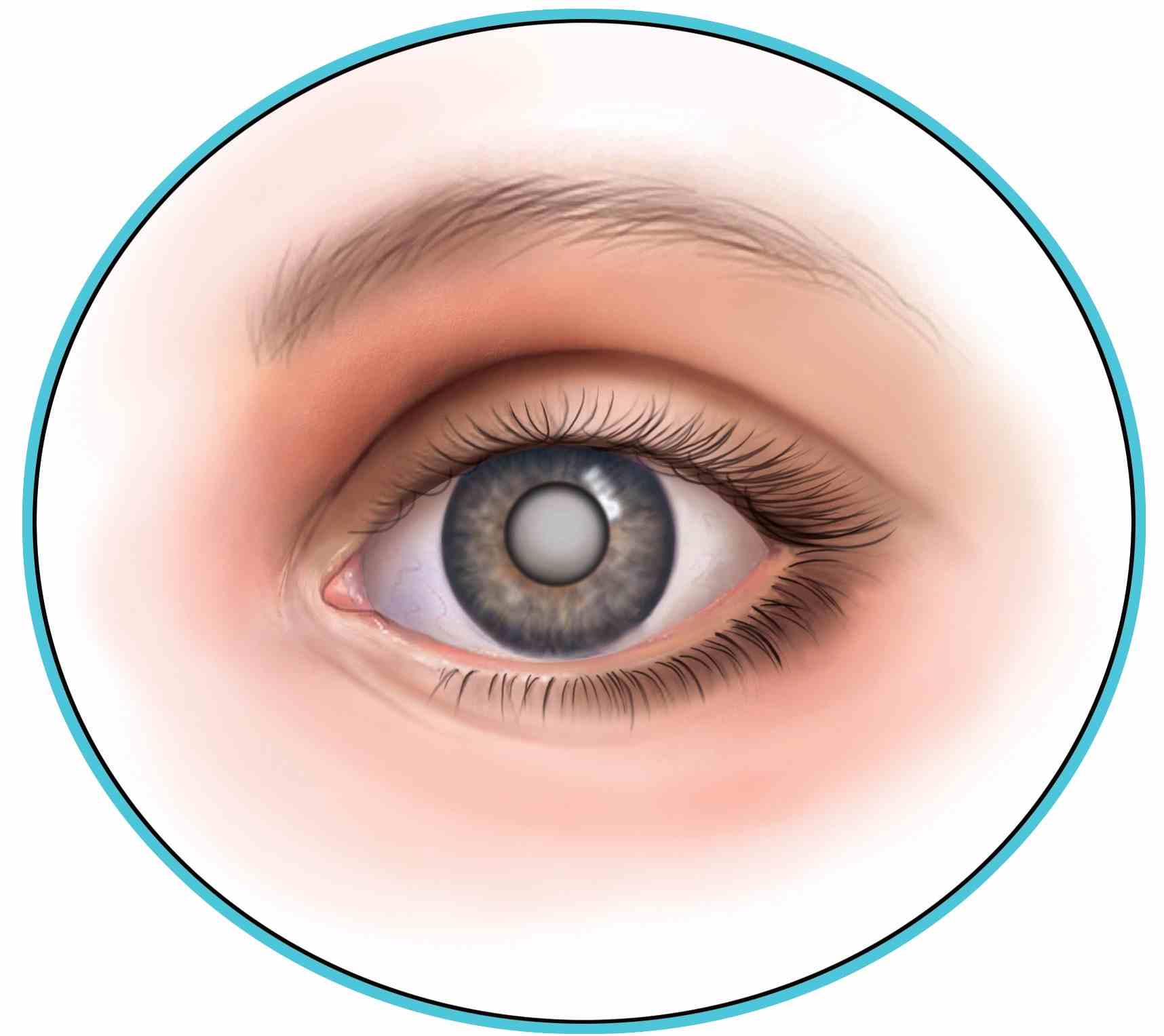
Conjunctivitis, also known as “pink eye,” is an inflammation of the conjunctiva (the membrane lining under the eyelids) and can be caused by allergies or infections. Allergic conjunctivitis and conjunctivitis caused by an infection can be hard to distinguish. Both have similar symptoms, such as redness, itching and swelling in the eye area. However, when conjunctivitis is caused by allergies, both eyes are usually affected. Viral or bacterial conjunctivitis can affect either a single eye or both eyes. It is important to pinpoint whether someone has conjunctivitis because of allergies or infection since each condition has a different treatment.
Common symptoms of allergic conjunctivitis are:
- Redness and itching under the eyelid
- Excessive watering
- Swelling of the eyeball
Common symptoms of conjunctivitis associated with infection are:
- Feeling that eyelids are glued shut upon waking
- Sensitivity to light
- Pus on the surface of the eye
- Burning sensation
Treatment
If you have ocular allergies or any other kind of allergic disease, the most effective treatment is prevention: try to avoid the allergens that trigger symptoms. For many, this is easier said than done, especially if your triggers are airborne, such as pollen. When ocular allergies can’t be controlled, there are several medications that may help relieve symptoms. Most of these treatments come in a topical form – such as eye drops or an ointment.
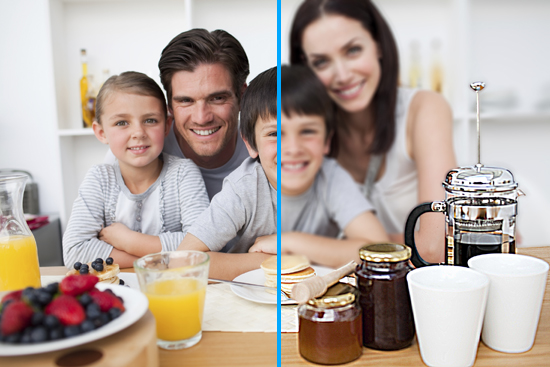
Eye drops, also called “tear substitutes,” can help in two ways: (1) by physically washing away allergens; and (2) by moistening the eye, which can become dry and red when irritated. Eye drops that contain medications to help reduce allergy symptoms are also available.
Topical Decongestants
Some eye drops contain topical decongestants that constrict small blood vessels and help reduce eye redness. These eye drops are available without a prescription. If you use eye drops with topical decongestants, be careful not to use them for prolonged periods. Overuse of topical decongestants can lead to increased swelling and redness that can last even after you stop using the drops. This is known as a “rebound effect.”
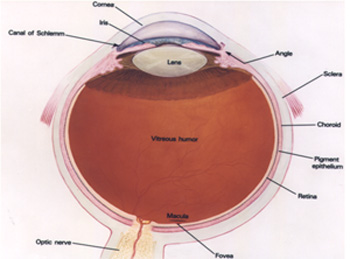
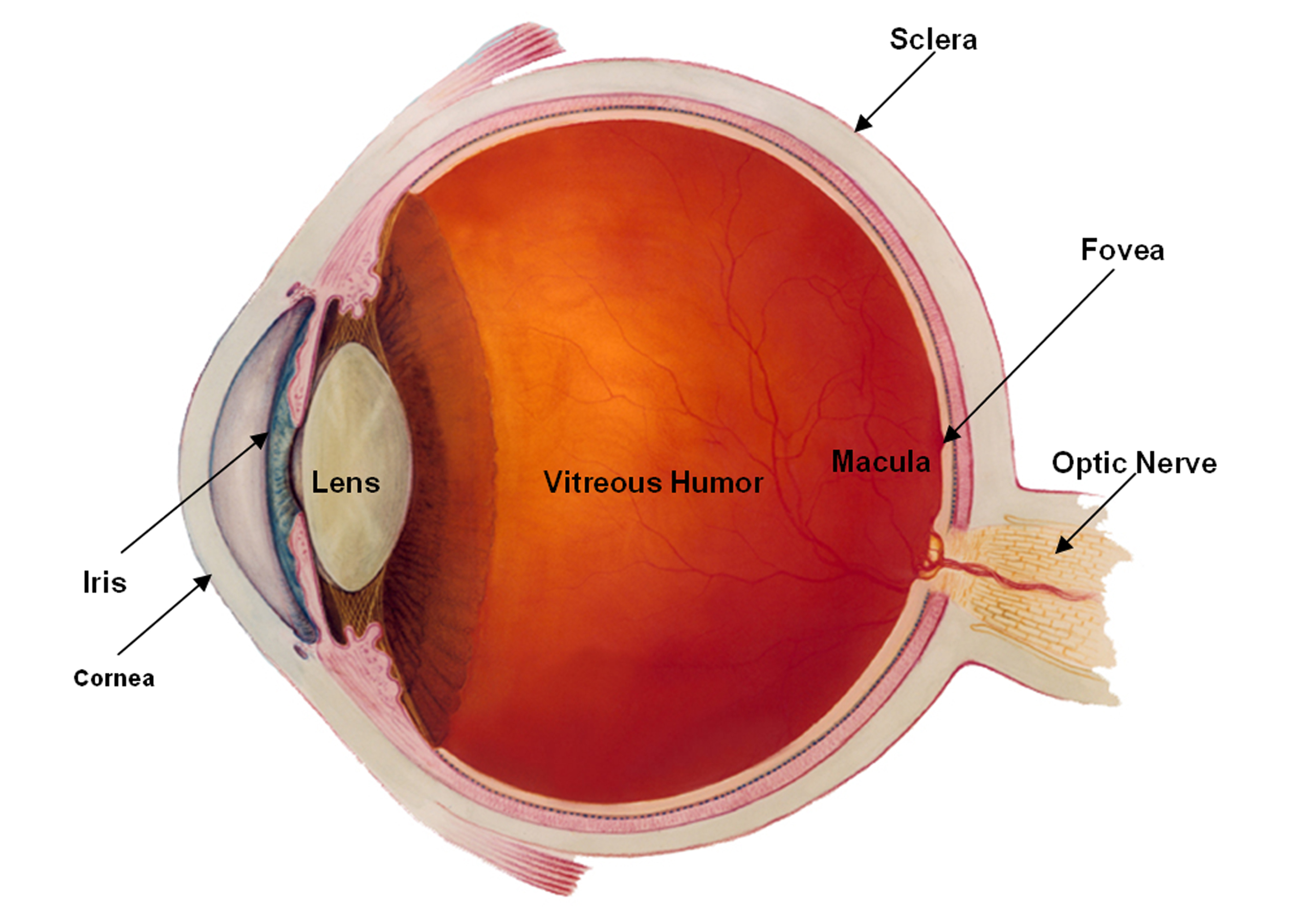
Topical decongestants, or any kind of eye drop containing chemicals that narrow blood vessels (called vasoconstrictors), shouldn’t be used if you have glaucoma. Glaucoma is damage to the eye that results from increased pressure in the eyeball (also called intraocular pressure, or IOP). Vasoconstrictors can worsen this condition.
Topical Antihistamines
Eye drops containing antihistamines can reduce redness and swelling in the eye. Antihistamines block the effects of the chemical histamine, which is responsible for allergic symptoms like swelling, redness and itching. Mild antihistamine eye drops are available over the counter, but stronger ones are available by prescription.
Helpful Strategies
Chilling any topical medications can help relieve redness and itching of the eyes. In addition, using cold compresses can help reduce some of the discomfort associated with conjunctivitis. A washcloth soaked in cold water works well. Oral non-steroidal anti-inflammatory drugs (NSAIDs), such as aspirin and ibuprofen-based medications, also can help reduce inflammation and symptoms like swelling in some patients.
Steroids
When topically administered medications like antihistamines and vasoconstrictors fail to help alleviate conjunctivitis symptoms, your doctor may prescribe topical steroids. Steroid eye drops can help control chronic and acute cases of conjunctivitis but should only be used as prescribed by your doctor. Steroids applied directly to the eye can cause a sharp increase in ocular pressure that can result in significant eye damage or glaucoma. Prolonged use of topical steroids in the eyes also can lead to cataracts. Cataracts form when the cornea on the surface of the eye gradually becomes opaque, causing blindness.
Because steroids can promote the growth of viruses, your doctor will want to rule out viral conjunctivitis as the cause of your eye problems before prescribing topical steroids.
Immunotherapy
Immunotherapy, also known as “allergy shots,” is another option for treating allergic conjunctivitis. Immunotherapy is a process that gradually desensitizes you to your allergens. Tiny amounts of the allergen are injected under the skin over the course of several years. During immunotherapy, your body will begin to develop a normal immune response to the allergen, and you won’t experience red, watery eyes every time you are around pets or pollen. Although immunotherapy may take several months to produce results, it can eventually greatly diminish the need for eye drops or other medication.